Section 4: Blood
Blood is a connective tissue whose matrix is fluid. It is composed of: red corpuscles, white cells, platelets, and blood plasma. It is transported throughout the body within blood vessels, which is the subject of Section 8 of this atlas.
Red Blood Cells
Red blood cells are also known as erythrocytes or red blood corpuscles. In humans, mature red blood corpuscles do not contain a nucleus and are therefore incomplete cells. They are incapable of cell division or reproduction and self-maintenance and have very little metabolic activity. Red corpuscles are usually biconcave discs, but they are flexible and can bend and fold depending upon specific circumstances as they circulate throughout the body. The biconcave shape favors the rapid absorption and release of oxygen and carbon dioxide by providing a large surface/volume ratio. Absence of a nucleus provides additional room for the carrier protein hemoglobin, which also facilitates respiratory function.
Circulating red blood corpuscles average about 8.0 µm., whereas in dried blood smears, they are approximately 7.5 µm. In fixed and sectioned tissues, they may shrink further, but they can still be used as a rough 6 µm for internal size estimation of cells and other structures because of their widespread histological availability. In human males, there are about 5.5 million red blood corpuscles per mm3 of blood. In females, the number is about 5.0 million per mm3. It has been estimated that a 150-pound (68.2 kg) human has about 5 liters of blood.
Massed red blood corpuscles are red in color owing to the presence of the respiratory pigment hemoglobin. Mature red blood corpuscles are membrane bound and normally devoid of a nucleus, nucleolus, cell organelles, and inclusions. A small number (about 0.5 to 1.5 percent) of immature but circulating red blood corpuscles (reticulocytes) contain some ribonucleoprotein (RNA) in the form of ribosomes. Because of their RNA content, they can be stained with nuclear dyes such as brilliant cresyl blue; the RNA will appear as a reticular network, hence the name reticulocyte. When their circulating number exceeds 1 per cent, an increase in oxygen-carrying capacity is indicated owing, perhaps, to hemorrhage, a change in altitude above sea level, or pathologic changes in the vital capacity of the lungs. It is well established that the life span of red blood corpuscles Is approximately 120 days. This means that about 25 X 1010 corpuscles are replaced daily, a turnover rate of 2.5 million per second. Both damaged and normal but "worn-out" erythrocytes are removed from the vascular system by macrophages, which are found primarily in the liver, spleen, and bone marrow. Breakdown products of hemoglobin are used in the formation of bile (bilirubin), and iron is conserved and used in new red cell production.
Red corpuscles, filled with a self-synthesized protein/iron complex, hemoglobin, carry carbon dioxide to the lungs from cells and tissues where it is exchanged for oxygen. The oxygen-carrying corpuscles are passively carried in blood plasma within blood vessels. Both exchanges, in tissues and lung, take place at the capillary level; this will be considered later. The cycle of gaseous exchange is repeated about 200,000 times during the life of the corpuscle. Red blood corpuscles, normally devoid of nucleic acids (DNA, RNA), stain with acid dyes because of their content of strongly basic hemoglobin. They stain red with the widely used hematoxylin and eosin (H. & E.) and other stains. The red corpuscle may therefore also be called eosinophilic or an erythrocyte ("red cell").
Since red cells are normally only found within blood vessels, any extravascular red cells may be an artifact of tissue preparation or the result of disease or a vascular accident (stroke).
White Blood Cells
White blood cells or leucocytes ("white cells") are complete cells because they contain a nucleus and other vital organelles. Two distinct types are recognized: (1) the so-called agranular leucocytes include lymphocytes and monocytes. These "agranular" leucocytes do not have cell type-specific granules. They are, however, not devoid of granules (as their name implies) but may contain varying numbers of azurophilic granules. (2) The granular leucocytes include neutrophiles, eosinophils, and basophils, each of which have their own type-specific granules from which they derive their names. Thus, the agranular leucocytes may or may not have nonspecific granules whereas the granular leucocytes always contain type-specific granules except in the earliest stages of their development.
The relative proportion of leucocytes in normal adult human blood (per mm3) is as follows:
-
Neutrophils-60 to 75 per cent, or 4200 to 5200/mm3
-
Eosinophils-1 to 3 per cent, or 70 to 21O/mm3
-
Basophils-0.5 to 1 per cent, 35 to 70/mm3
-
Lymphocytes-20 to 45 per cent, or 1400 to 3150/mm3
-
Monocytes-2 to 10 per cent, or 140 to 700/mm3
The average number of leucocytes in a normal adult varies between 5000 and 9000 per mm3. The number of white blood cells is increased (above 12,000) or decreased (below 5000) in disease states. An increase over the normal values is termed leucocytosis; a decrease is termed leucopenia. As examples, neutrophils are known to increase in number in bacterial (pus-forming) infections, eosinophils increase in allergic conditions and parasitic infections, and basophils may increase in certain inflammatory conditions of skin. Other diseases may result in changes in the number of more than one type of leucocyte.
The life span of white blood cells is considered to be shorter than that of red blood cells. The exact life span is, however, not known, because these cells normally leave the vascular system to enter tissue spaces to perform their special functions. Aging leucocytes are removed from the circulation by macrophages located in the liver and spleen. They may die and disintegrate in the connective tissue with remnants being phagocytized by histiocytes, or they may migrate through the epithelium of the gastrointestinal and respiratory tracts and be eliminated.
Some leucocytes can be recognized in tissue sections, but others are not seen to advantage by this method. A peripheral blood smear is the preferred method for identification of blood cell types. In this method, a drop of blood is spread thinly and evenly over a microscope slide. The thin layer of blood air- dries rapidly, is fixed with methanol, and stained with a Romanovsky stain. Romanovsky (1891) discovered that certain dye mixtures stained blood cell components in a way that permitted accurate determination or differential counts of the variety of cells in the circulating blood and bone marrow. Some white cell cytoplasmic components (primarily inactive DNA and RNA) stain blue with methylene blue (hence, they are called basophilic), some (primarily lysosomes and a variety of other hydrolytic enzymes) may bind the azures (dye products of methylene blue oxidation) and appear light purple; some (primarily hydrolases, which digest phagocytized materials such as antigen-anti body complexes) may bind eosin (hence, they are called eosinophilic or acidophilic), and some (primarily hydrolytic enzymes related to phagocytic function) may bind another dye complex, which produces a dusty-pink or violet color (and are called neutrophilic, in spite of the fact that the particles are not chemically neutral). In this atlas, we have elected to use Wright's stain, which is classified as a Romanovsky-type stain. Giemsa's stain is also widely used and will be similar in its staining characteristics. Leucocytes are relatively inactive while being passively carried in the blood stream, but, because they are capable of ameboid movement, they concentrate in sites of infection and are always found in sites of "potential infection" in tissues and organs; the particular vulnerability of the diges tive system has already been mentioned. Neutrophils and monocytes are the most phagocytic of the white blood cells; they ingest foreign particles, bacteria, and degenerating cells and cell fragments whether or not they can digest them. Monocytes are considered to be the most active phagocyte. Neutrophils provide the first line of defense against invading foreign bodies and organisms, and lymphocytes are believed to form antibodies, a function shared with plasma cells.
Agranulocytes
Lymphocytes
Lymphocytes vary widely in size. Small lymphocytes are 7 to 10 µm in diameter, and large lymphocytes are approximately 14 to 20 µm in diameter, although intermediate sizes may be encountered. Larger lymphocytes are thought to be involved in humoral immunity, because they are activated by specific antigens; they differentiate into B lymphocytes and are formed in specific areas of the spleen and lymph node. Most (80 per cent) of the lymphocytes, however, are T lymphocytes, which are long- lived and are formed in different areas of the spleen and lymph node than are the B lymphocytes.
The nuclei of lymphocytes are usually round but may be slightly indented. Nuclear chromatin is clumped, inactive heterochromatin, which stains intensely with Wright's stain. The cytoplasm immediately adjacent to the nucleus is agranular and poorly stained and appears as a perinuclear halo. The thin rim of remaining cytoplasm is usually intensely basophilic but may stain variable shades of blue. Some lymphocytes possess a few azurophilic granules, but they are not evenly distributed. Lymphocytes are produced in lymphold tissues, which are discussed in Section 9.
Monocytes
Monocytes are approximately 15 to 25 µm in diameter. The nuclei of monocytes are usually kidneyshaped, indented, or lobed. The cytoplasm of monocytes is gray-blue and contains azurophilic granules, which are generally evenly distributed. Vacuoles are often demonstrable in the cytoplasm. Monocytes frequently show evidence of ameboid movement and are voracious phagocytes. Monocytes are also produced in lymphoid organs
Granulocytes
The granulocytes include the neutrophils, eosinophils, and basophils. These cells are also known as polymorphonuclear cells because of their characteristic segmented nucleus. The three polymorphonuclear cell types are produced in the bone marrow.
Neutrophils
Neutrophils constitute 60 to 70 per cent of circulating white blood cells. They are 12 to 15 µm in diameter and possess a characteristic segmented nucleus with two to five lobes joined by fine strands of chromatin, hence the name polymorphonuclear neutrophils (PMN). The stainable heterochromatin is inactive DNA; there are no nucleoli. Immature "polymorphs" have a non-segmented oblong or rectangular nucleus; hence they are called bands. They are often bent and look like horseshoes, but they never bear this name. In females, the X chromosome may appear as a "drumstick-like" appendage on one of the lobes of the nucleus Neutrophils have abundant cytoplasm with two types of granules of different size and staining characteristics. When stained with Romanovsky-type stains, the cytoplasm appears a dusty-rose color because of cell type-specific granules that are near and below the resolving power of the light microscope (about 0.2 µm). The granules contain several enzymes: alkaline phosphatase, collagenase, and lysozyme. The second population of granules are not cell-specific. They are azurophilic, about 0.5 µm in diameter, and stain metachromatically (light purple or violet). These are primary lysosomes rich in enzymes. Although not seen with the light microscope, these cells have few mitochondria and utilize anaerobic pathways to degrade glycogen for their energy requirements. Neutrophils survive 1 to 4 days in tissues once they leave the blood stream. They traverse the connective tissues by ameboid movement and are the most active phagocytes of the three granulocytes. The azurophilic granules or lysosomes are capable of hydrolyzing bacteria, cellular debris, fungi, and viruses. Ameboid movement and, to a lesser degree, phagocytosis is seen in eosinophils and basophils.
Eosinophils
Eosinophils constitute 2 to 4 per cent of circulating white blood cells. The cell is 12 to 15 µm in diameter and usually has a bilobed nucleus. The cell is easily identified by the presence of many (about 250) large and refractile cell-specific granules. These stain red with Romanovsky-type stains. The granules stain with the dye eosin; hence, the name eosinophil, which means "eosin-loving." In the eosinophil, unlike the neutrophil, specific granules are primary lysosomes.
Basophils
Basophils constitute less than 1 per cent of the circulating white blood cells and usually require patient examination of a blood smear to locate, but they are worth the search when found. They are 12 to 15 µm in diameter but may be smaller. They possess an irregularly lobed nucleus most often obscured by the large, metachromatically basophilic granules; hence, the name basophil. The specific granules are irregular in size and shape and stain metachromatically owing to the presence of heparin. They also contain histamine.
Cell Type
Size (µm)
Number (mm3)
Function
Neutrophil
12-15
300-700
Phagocytosis (cellular debris, bacteria, fungi, viruses, etc)
Eosinophil
12-15
120-400
Phagocytosis (antigen -antibody complexes), antiparasite agents
Basophil
12-15
30-100
Immediate hypersensitivity reaction
Platelets
Blood platelets are fragments of the cytoplasm of megakaryocytes. Platelets are small discs about 2 to 4 µm in diameter and number between 200,000 to 350,000 per mm3 of blood. In general, two to six blood platelets or thrombocytes are seen in an oil immersion field, but their distribution is variable and they may appear in large clumps. Their specific function is related to the clotting of blood both inside and outside blood vessels.
Blood Plasma
The fluid in which the blood cells reside (when within blood vessels) is called blood plasma. Plasma constitutes 55 per cent of whole blood, whereas the cellular components total 45 per cent in a normal hematocrit determination. Blood plasma contains gases, proteins, carbohydrates, amino acids, lipids, inorganic salts, enzymes, hormones, and antibodies (immunoglobulins). It is slightly alkaline. Blood plasma serves an important role in coagulation, temperature regulation, respiration, regulation of blood pH (as a buffer), and fluid balance. Hormones, absorbed nutrients, and metabolic wastes are carried in the plasma to sites of action, utilization, or elimination. When blood plasma clots, the remaining fluid is called blood serum.
Origin of Blood Cells
Since blood cells have a short life span, they must be constantly replaced in vast numbers. The term applied to this process is hematopoiesis and takes place in the bone marrow and lymphoid tissues of adults. In the embryo and fetus, various organs are active in hematopoiesis, including the yolk sac, liver, spleen, thymus, and lymph nodes, as well as bone marrow.
Erythropoiesis
Red blood corpuscles undergo their maturation within bone marrow, and several "stages" can be recognized The earliest cells of this series have a large round nucleus, reticulated chromatin, and one or more small nucleoli. The cytoplasm is seen as a thin rim, which stains a royal blue color with Wright's stain. These cells, unfortunately, are called by several names of which you should be aware but not memorize. Determine the nomenclature preferred by your instructor and then underline the name to simplify the learning process; for example, rubriblast, proerythroblast, pronormoblast, or megaloblast. As the rubriblast matures, the nucleus becomes smaller, chromatin coarsens, and nucleoli become ill defined or disappear. The cytoplasm remains basophilic and stains blue. These cells are termed prorubricytes, basophilic erythroblasts, basophilic normoblasts, or early erythroblasts. The next recognizable stage involves further coarsening and reduction of nuclear size. Nucleoli are absent. Relatively, the cytoplasm appears to occupy more of the cell and is seen to contain a mixture of eosinophilic (red) and basophilic (blue) purplish cytoplasm. These cells are named rubricytes, polychromatophilic erythroblasts, normoblasts, intermediate erythroblasts, or intermediate normoblasts. The nucleus of the next stage is still smaller than the preceding stage and is a solid blue-black color. The nucleus is now non-functional and ready to be discarded. The cytoplasm is predominantly acidophilic with some residual basophilia. The hemoglobin, which is eosinophilic, dominates with only minimal amounts of residual ribonucleoprotein staining the cytoplasm a purplish tint. The nucleus is ejected from the cell in the next "stages" and the cytoplasm still retains a very slight purple tint, signifying the increased synthesis of hemoglobin. These cells are termed diffusely basophilic erythrocytes or polychromatophilic erythrocytes. In the final "stage,ff the cytoplasmic ribonucleoprotein disappears and the corpuscles appear as flexible biconcave discs, 6 to 8 µm in diameter, and reddish in color when stained with Romanovsky-type stains; in this atlas, with Wright's stain.
Granulocytic Series
Granular leucocytes )develop in the bone marrow from undifferentiated cells called myeloblasts. Myeloblasts are approximately 20 µm in diameter. The nucleus is round, stains a purple color, and contains two or more nucleoli. The cytoplasm is basophilic, and, when stained with Wright's stain, it appears agranular and pale blue. In the next recognizable "stage," the nucleus is reduced in size and the chromatin becomes more coarse and unevenly stained. This cell now contains the granules that stain variably from red to purple-blue and is designated a progranulocyte or a promyelocyte. A progranulocyte becomes a myelocyte when the granules become sufficiently differentiated in size, color, and shape to be positively identified as the specific granules of neutrophils, eosinophils, or basophils. The subsequent developmental "stages" are identical for the three types of granulocytes or polymorphonuclear cells.
The primary changes include a reduction in cell size and alterations in nuclear shape. The nucleus of the myelocyte tends to be slightly flattened. The chromatin becomes increasingly coarse, and nucleoli are usually indistinct or absent. The next stage, the metamyelocyte, contains an indented kidney-shaped nucleus. Additional folding results in a horseshoe-shaped nucleus, which stains deeply with basic dyes. The overall cell size continues to decrease. These cells are called "bands." The final developmental 11stageff results in a cell with a segmented or lobed nucleus, the lobes being united by narrow filaments or strands of chromatin. The cytoplasm contains the specific granules characteristic of the three types. These cells are called segmented granulocytes or polymorphonuclear granulocytes. The mature polymorphonuclear granulocyte is approximately 15 µm in diameter.
All lymphocyte progenitor cells are believed to originate in the bone marrow. They leave the marrow to develop in the thymus to form T lymphocytes, which will leave the thymus to populate other lymphoid organs. Other bone marrow lymphocyte progenitor cells become B lymphocytes, which leave the marrow to populate other specific areas of lymphoid tissue. T and B lymphocytes cannot be distinguished by ordinary histologic methods. See Section 9.
WHITE BLOOD CELLS
Granulocytes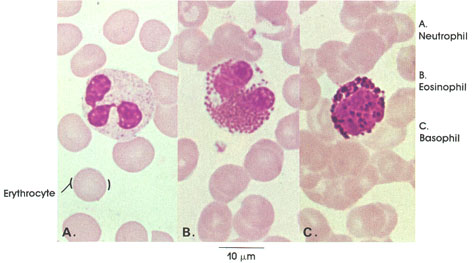 Human, air-dried blood smear, Wright's stain, 1416 x.
Human, air-dried blood smear, Wright's stain, 1416 x.
Erythrocyte: Usually biconcave and circular outline, devoid of a nucleus. Number in man varies between 5 and 5.5 million per cubic mm of blood. Erythrocytes carry oxygen from the lungs to the tissues and carbon dioxide from the tissues to the lungs.
Neutrophil: Compare sizes of the neutrophil and the erythrocyte. Lobulated nucleus, individual lobes connected by thin bridges. Cell type-specific cytoplasmic granules are small. Neutrophils constitute 40 to 75 per cent of the total white blood cell count. The number of neutrophils increases in inflammation, and they act as the first line of defense against invading pyogenic organisms.
Eosinophil: Nucleus bilobed. Cell type-specific cytoplasmic granules are large and uniform in size and stain intensely red with acid dyes. They constitute 1 to 3 per cent of total white count and increase in number in allergic states and in parasitic infections.
Basophil: The nucleus is large but less lobulated than other white blood cells. Cell type-specific cytoplasmic granules are large and variable in size and have a strong affinity for basic dyes. They constitute 0.5 to 1 per cent of white count and are believed to synthesize the heparin and histamine found in circulating blood.
LYMPHOCYTES
Small and large lymphocytes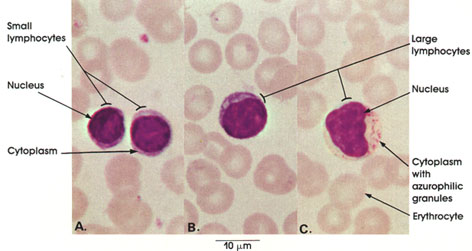 Human, air-dried blood smear, Wright's stain, 1416 x.
Human, air-dried blood smear, Wright's stain, 1416 x.
Small lymphocytes: These are the most common type in normal blood. They have a large, dense, round nucleus and thin basophilic cytoplasm and are capable of ameboid movement and the production of antibodies.
Large lymphocytes: These are not very common in normal blood. The nucleus is indented, and cytoplasm is more abundant than in small lymphocytes. Azurophilic granules are frequently found in large lymphocytes; they are less commonly detected in small lymphocytes
MONOCYTES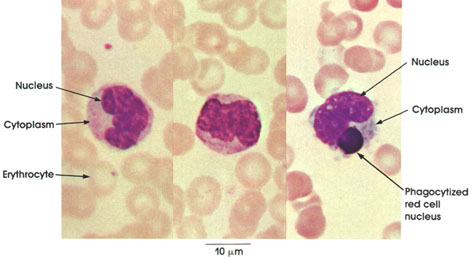 Human, air-dried blood smear, Wright's stain, 4416 x.
Human, air-dried blood smear, Wright's stain, 4416 x.
Monocytes are the largest cells found in normal blood. The nucleus is centrally or peripherally located, indented, and ovoid or horseshoe-shaped; the nuclear chromatin is not as dense as that of lymphocytes. Cytoplasm is abundant and contains azurophilic granules, which are usually smaller than those seen in lymphocytes. Monocytes are voracious phagocytes. The monocyte seen on the extreme right shows pseudopodia extending from the cell body and contains a phagocytized red cell nucleus
Note the comparative size of erythrocytes and monocytes.
BONE MARROW
PERIPHERAL BLOOD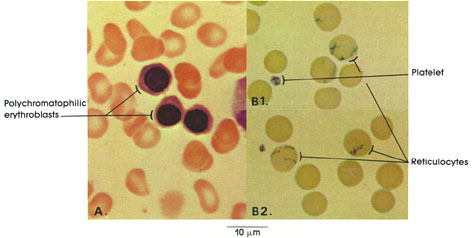 A. Human, air-dried marrow smear, Wright's stain, 1416 x.
A. Human, air-dried marrow smear, Wright's stain, 1416 x.
B. Human, air-dried blood smear, brilliant cresyl blue, 1416 x.
Polychromatophilic erythroblasts (rubricytes): Derivatives of basophilic erythroblasts (prorubricytes). Dense nuclear chromatin with polychromatophilic cytoplasm owing to a declining RNA content and an increase in newly synthesized hemoglobin.
Reticulocytes: Immature red blood cells seen in the circulating blood. Clumping of ribosomes gives them a reticulated appearance.
Platelets: Also called thrombocytes, these are minute round or ovoid structures. They are important in blood coagulation and are derived from bone marrow megakaryocytes.
RED BONE MARROW
In situ
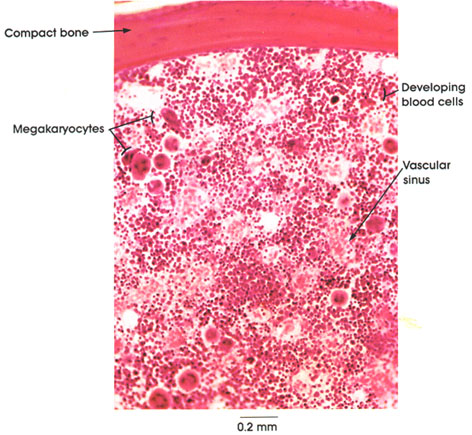
Human, Müller's fluid, H. & E., 50 x.
In this plate, a layer of compact bone surrounds the red bone marrow cavity.
Red or hemopoietic marrow is the characteristic variety of marrow until middle childhood. By late adolescence, most red marrow is replaced by fatty or yellow bone marrow. In adults, red marrow occurs in the sternum, ribs, vertebrae, heads of long bones, and cranium.
Red marrow is characterized by high cellularity and sinuses filling spaces between a delicate reticular supporting tissue. The cells seen are giant megakaryocytes and developing red and white blood cells.
BONE MARROW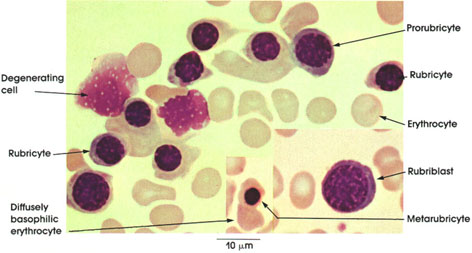 Human, air-dried marrow smear, Wright's stain, 1416 x.
Human, air-dried marrow smear, Wright's stain, 1416 x.Rubriblast (proerythroblast, hernocytoblast, myeloblast): Stem cell of the erythroid series with a large rounded nucleus, basophilic cytoplasm.
Prorubricyte (basophilic erythroblast): This develops from the rubriblast. It is smaller than the stem cell, and the nucleus has coarser chromatin. RNA-rich cytoplasm is densely basophilic. Basophilia obscures hemoglobin content. It undergoes mitotic division, giving rise to rubricytes.
Rubricyte (polychromatophilic erythroblast): This is a product of mitotic division of prorubricytes and is smaller than the mother cell. Nuclear chromatin more compact. Cytoplasmic basophilia are less marked and hemoglobin content is greater than in the mother cell. Rubricytes have an affinity for both acid and basic dyes (because of their content of hemoglobin and RNA respectively), which determines their polychromatophilic staining characteristics.
Metarubricyte (normoblast): It arises by mitotic division of the rubricyte. The nucleus is small and pyknotic. Cytoplasm is distinctly aciclophilic owing to increased hemoglobin content.
Erythrocyte: Non-nucleated (nuclei of metarubricytes have been extruded) with circular outline. In side view, they appear dumbbell-shaped because of the biconcave nature of their surfaces. The number varies in man from 5 to 5.5 million per cubic mm. They carry oxygen from lungs to.tissue and carbon dioxide from tissue to lungs, and are filled with hemoglobin. immature stages in development (reticulocytes) have a diffusely basophilic cytoplasm because of the residual content of RNA.
Degenerating cell: Often found in bone marrow. They are remnants of damaged corpuscles, megakaryocytes, or myeloblasts. These are primarily artifacts of a marrow smear preparation.
BONE MARROW
Developing neutrophils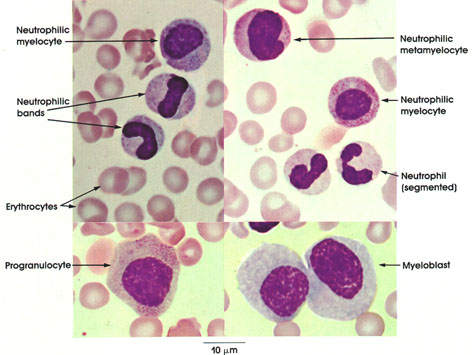 Human, air-dried marrow smear, Wright's stain, 1416 x.
Human, air-dried marrow smear, Wright's stain, 1416 x.
Myeloblast: The stem cell of the leucocytic series with lightly basophilic cytoplasm. The nuclei are large and rounded. The chromatin is in the form of moderately coarse interconnected strands. They constitute 0.3 to 0.5 per cent of marrow cells. Myeloblasts increase in leukemia.
Progranulocyte: Also called promyelocyte. It arises and differentiates from myeloblasts. It has large cells; its nuclei are rounded with coarse chromatin. Cytoplasm is basophilic with some azurophilic granules. This cell type constitutes about 4 per cent of marrow cells.
Neutrophilic myelocyte: This arises from progranulocytes. It is smaller, has less basophilic cytoplasm containing differentiated granules and a nucleus with more compact chromatin.
Neutrophilic bands: These are immature neutrophils. The nuclei are horseshoe- or drumstick-shaped.
Neutrophilic metamyelocyte: It has a kidney-shaped nucleus and is not capable of division. It differentiates into mature neutrophilic myelocytes.
Neutrophil (segmented): This is a mature cell. Its nucleus is markedly lobulated. The lobules may be connected with a thin chromatin thread. Chromatin is compact, and there is abundant cytoplasm. Granules in the cytoplasm are small and may be inconspicuous.
BONE MARROW
Developing eosinophils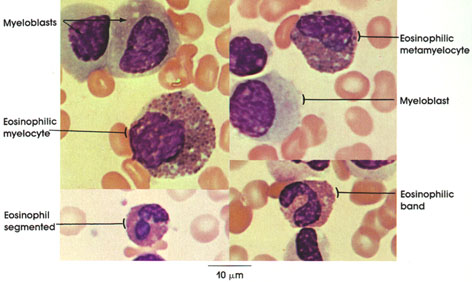 Human, air-dried marrow smear, Wright's stain, 1416 x.
Human, air-dried marrow smear, Wright's stain, 1416 x.Myeloblast: Stem cell of the leucocytic series. It has a rounded large nucleus and lightly basophilic agranular cytoplasm. .
Eosinophilic myelocyte: These develop from myeloblasts. Specific acidophilic granules appear in cytoplasm. The nucleus is rounded or oval. Chromatin of nucleus is coarser than in the myeloblast. This cell is capable of division.
Eosinophilic metamyelocyte: This cell is no longer capable of cell division. The nucleus is kidney- shaped or indented. Cytoplasm contains acidophilic granules.
Eosinophilic band: Immature or juvenile eosinophil. The nucleus is horseshoe- or drumstick-shaped, and there are eosinophilic granules in cytoplasm.
Segmented eosinophil: Mature eosinophil. The nucleus is lobulated and the lobes are connected with thin chromatin threads. There is abundant granular cytoplasm.
BONE MARROW
Developing basophils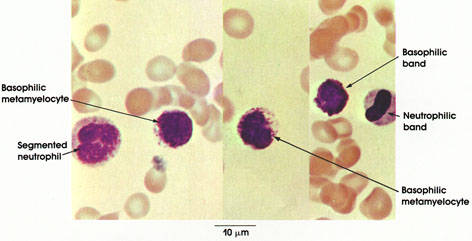 Human, air-dried marrow smear, Wright's stain, 1416 x.
Human, air-dried marrow smear, Wright's stain, 1416 x.
Basophilic metamyelocyte: Derived from basophilic myelocyte, which is not represented in this figure. Basophilic myelocytes are scarce and may not be seen in a single marrow smear preparation. It is believed that their granules are water soluble. This cell is no longer capable of cell division. The nucleus is oval to kidney-shaped. Cytoplasm has basophilic granules.
Basophilic band: An immature basophil with a horseshoe-shaped nucleus. There are basophilic granules in the cytoplasm.
BONE MARROW
Wandering cells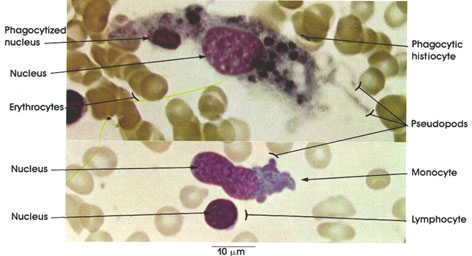 Human, air-dried marrow smear, Wright's stain, 1416 x.
Human, air-dried marrow smear, Wright's stain, 1416 x.
Phagocytic histiocyte: Large cell. Irregular cell outline with many short cell processes (pseudopods). There is abundant cytoplasm containing phagocytized material. The nucleus is oval.
Monocyte: Large cell with a prominent eccentric nucleus. It has a highly ameboid cytoplasm containing various inclusions.
Lymphocyte: Spherical, dense nucleus with a thin, inconspicuous rim of basophilic cytoplasm
BONE MARROW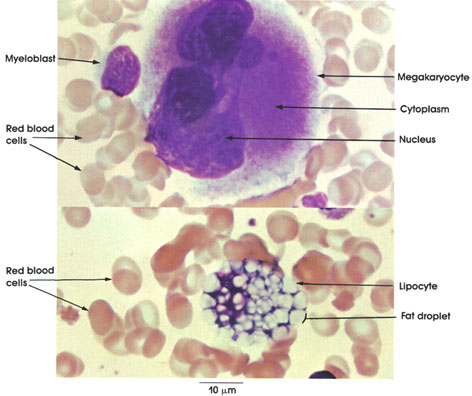 Human, air-dried marrow smear, Wright's stain, 1416 x.
Human, air-dried marrow smear, Wright's stain, 1416 x.Megakaryocyte: Giant cell characteristic of bone marrow, with a conspicuous multilobed nucleus. Cytoplasm contains fine granules. Pseudopodia extend from the cell surface and later detach to form the blood platelets. Blood platelets participate in the blood-clotting mechanism by contributing to the formation of thromboplastin, by "plugging" abnormal breaks in the endothelium of blood vessels, and by inducing the constriction of damaged blood vessels.
Red blood cells: Non-nucleated corpuscles having a circular or dumbbell-shaped appearance. Contain hemoglobin.
Lipocyte: Fat cells are constantly present in bone marrow. They have irregular outlines and are filled with lipid droplets.